Cutting Off Health Insurance for Eligible Kids During the “Unwinding” of Continuous Coverage Disrupts Access to Medications, Cancer Treatment, Mental Health Support, Immunizations and More
Texas is in the process of reviewing Medicaid eligibility for 5.9 million Texans as part of the “unwinding” of Medicaid rules that allowed Medicaid enrollees to maintain their health insurance without renewing it during the pandemic. Texans who are no longer eligible should be removed from Medicaid and — if they do not have other health insurance — transferred to another program for which they qualify, such as the Children’s Health Insurance Program (CHIP), Healthy Texas Women, or HealthCare.Gov. Texans who are still eligible should remain enrolled.
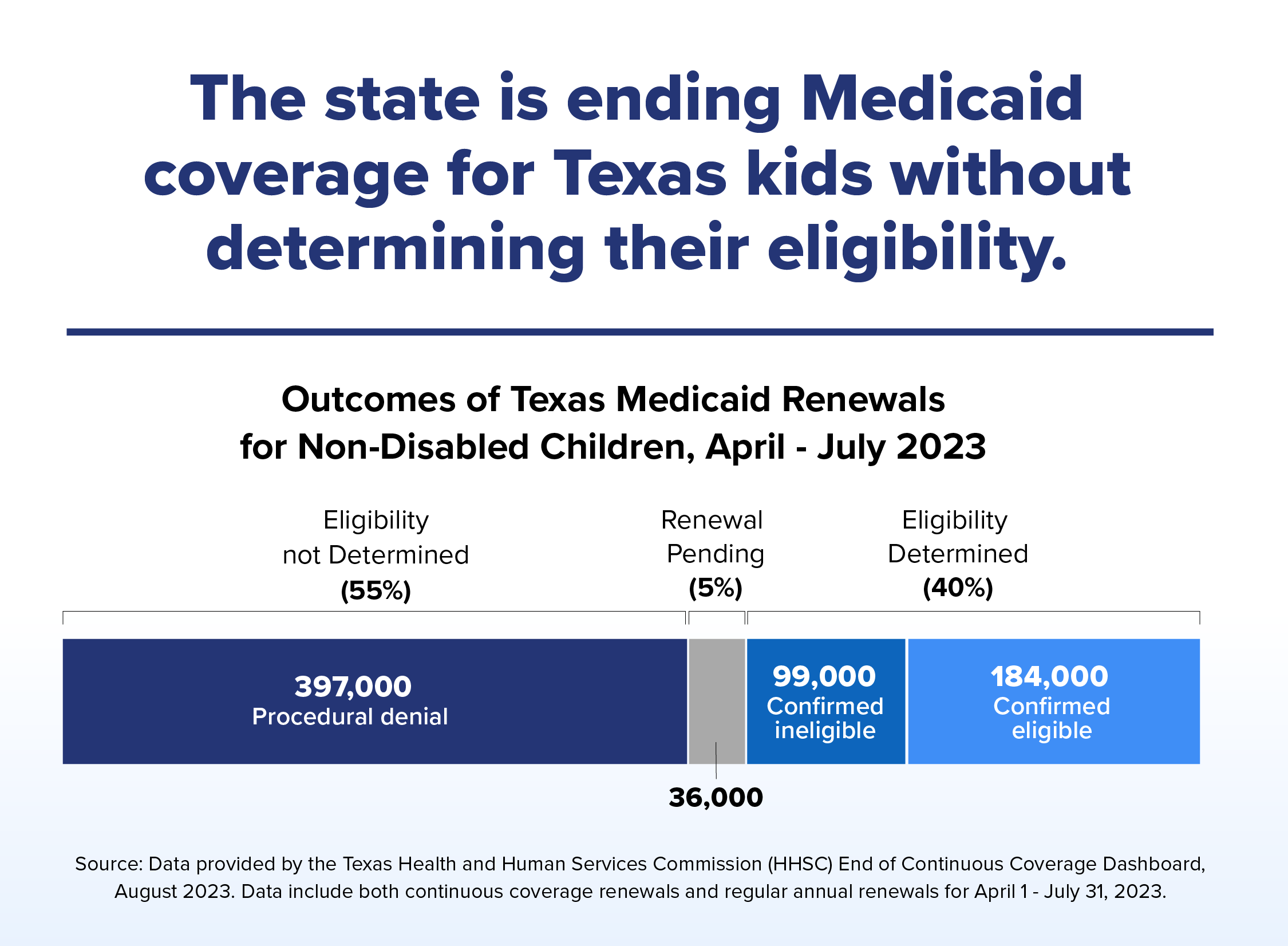
In August, HHSC released cumulative data on Medicaid renewals from April 1 through July 31. Unfortunately, the data revealed that, in most cases, the state is not successfully determining who is eligible and who is not — but is often cutting off Medicaid health insurance anyway. The vast majority of those removed from Medicaid insurance were children.
Our new four-page policy brief breaks down the data, explains what comes next, and offers key policy recommendations to state leaders.