New state data indicate that the Texas Medicaid enrollment system is not working in an efficient, orderly, and timely manner — and that has real consequences for Texas kids.
Texas has finished reviewing Medicaid eligibility for 5.9 million Texans as part of the “unwinding” of Medicaid rules that allowed enrollees to maintain their health insurance without renewing it during the pandemic.
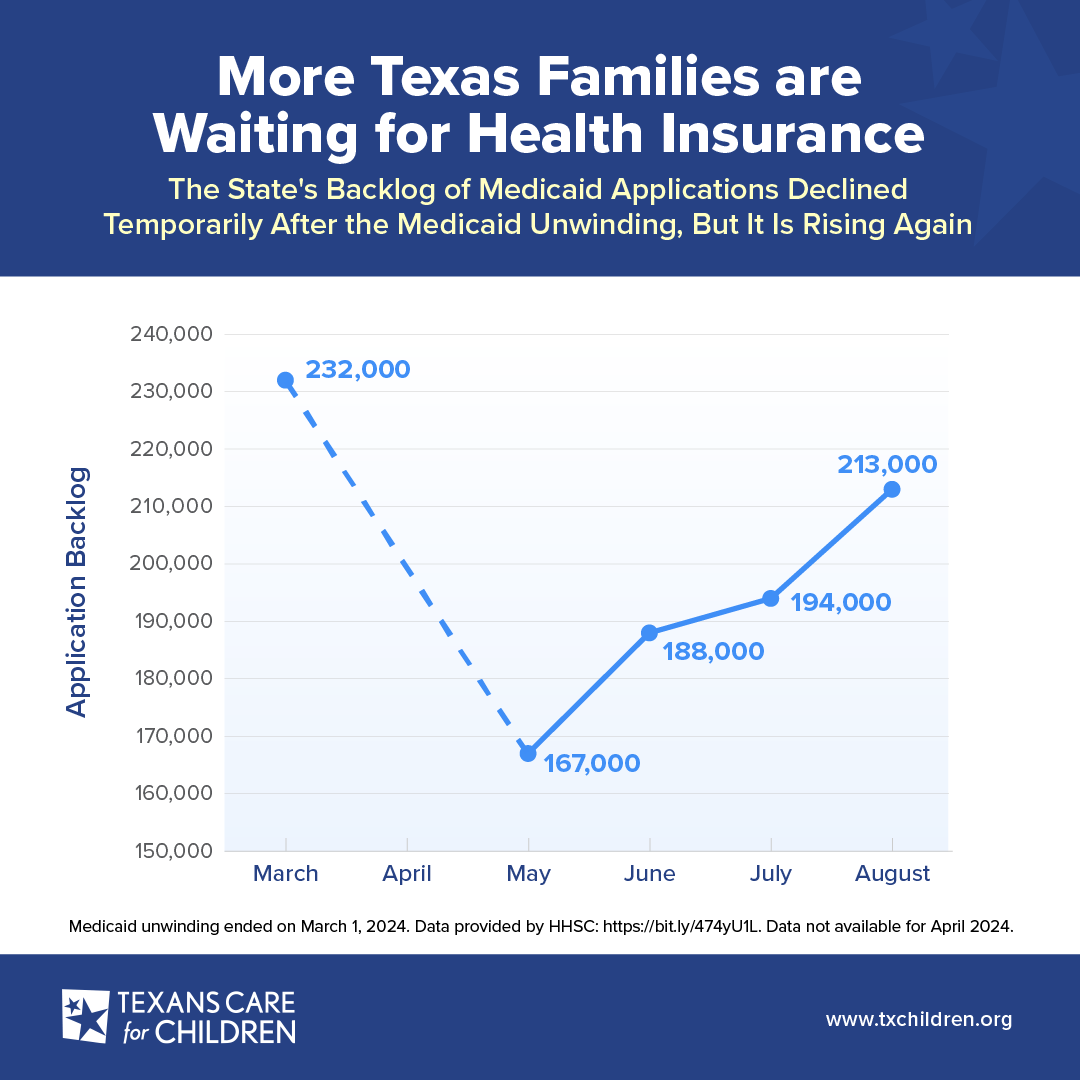
We expected that with the unwinding over, the state’s backlog of Medicaid applications would start improving. Unfortunately, that is not the case. Instead, after a temporary improvement in the backlog, more and more Texas kids are waiting for health coverage.
The state publicly shares this and other Medicaid information regularly through stakeholder calls. According to their data, the state’s backlog for processing Medicaid health insurance applications is back up to 212,745 in August after dropping to 167,000 in May.
This means 212,745 Texas families have filled out applications for Medicaid health insurance for their kids — but the state has not even started processing them. On average, these families are waiting three to four months to get connected to health insurance.
While families are waiting, we’re concerned about children who won’t be ready for school because they are waiting on checkups, immunizations, physical therapy for disabilities, medications to keep them healthy, mental health treatment, and other care because they are waiting for health coverage.
When eligible kids are able to enroll in Medicaid health insurance, we know there are many benefits. We recently spoke with several families about their positive experience with Medicaid insurance. Lola, for example, was able to get the surgeries she needed after she was born and, when she was older, get back to school when she was out sick. The challenge is making sure that other eligible kids are able to enroll without facing long delays.
Why are there persistent delays? The Texas eligibility system is overly reliant on state eligibility workers instead of maximizing technology.
The state has invested energy and resources into filling eligibility worker vacancies, reducing turnover, and encouraging overtime. The Texas Health and Human Services Commission (HHSC) reduced the vacancy rate for eligibility advisors from 21.2% in March 2022 to 2.5% in April 2024, and overtime has been required for the last year. Despite the increased staffing, the backlog of applications continues to grow.
It’s clear that just focusing on staffing will not solve the backlog problem. If Texas leaders want to tackle the backlog to ensure kids get the health coverage they need, it’s time to upgrade technology to streamline the state’s eligibility system.
Texas needs a more efficient, accurate approach to Medicaid/CHIP enrollment that reduces delays and increases the use of smart, data-driven processes. We urge the Texas Legislature to prioritize the following policies next legislative session:
- Improve the efficiency of data-driven renewals — also known as ex parte renewals — by fully leveraging reliable third-party data sources. For example, the state should allow for broader use of Texas Workforce Commission (TWC) wage data to more efficiently and accurately re-verify Medicaid eligibility.
- Notify parents when their child is eligible for Medicaid or CHIP based on already verified data for SNAP.
- Invest in technology upgrades for the Medicaid eligibility and enrollment system.
We look forward to working with legislators, HHSC staff, families, and other interested Texans to make these important changes to our Medicaid program so families can take their kids to the doctor when they’re sick and get back to school.